|

Is it common for IBS to strike with gastric pain as well?
Gastric pain has different meaning for different people. For many doctors, 'gastric' is often used to describe any pain in the upper part of the abdomen or any pain in relation to a meal. The term 'gastric' is also used to imply that the pain is produced by stomach acid. Conditions in which stomach acid plays an important role are gastric ulcer, duodenal ulcer and acid reflux. However, many people experience pain from the stomach that is not due to acid. One way to suspect this is when a person's pain is not improved after taking medications that reduce or neutralise acid. Both patients and doctors often confuse IBS pain as 'gastric' pain. For example, we have found that about 20-50% of patients referred by their doctor of having 'gastric' pain, actually had IBS or a related condition called functional dyspepsia. Both IBS and functional dyspepsia have more to do with disturbances in the movement and sensations of the intestines and stomach, rather than acid irritation. About 50% of people with IBS point to the so-called 'gastric' area as the site of pain. IBS pain is very often worse after eating. Many people with IBS will also experience bloating. The key is to pay close attention to your bowel movements - does passing motion make the pain better, do you observe a change, no matter how slight it may be, in the frequency or consistency of the stool on the day that you have pain.
Bloating & Constipation
Is it safe to use herbal slimming and detox tea to improve bowel movements?
Many herbal slimming detox teas and even Chinese medicine teas contain a laxative ingredient known as senna. Senna forms the basis for a common over the counter laxative known as Senokot. I believe that part of the reason why a laxative is often included in these teas is that clearing the bowels does help to make a patient feel less bloated. Furthermore, popular health fads try to promote the idea that purging helps to clear toxins from the body. However, mainstream science does not support the concept of detoxification except in very limited circumstances such as liver cirrhosis or liver failure.
While senna is generally safe, having diarrhea on a frequent basis is not. Frequent purging can lead to dehydration and electrolyte depletion which can be harmful for the kidneys and the heart. Another common side effect of senna-type laxatives is the development of a brown discolouration of the intestinal lining instead of the healthy pink colour. Although this brown discolouration otherwise known as melanosis coli may not be harmful, it is certainly not normal.

Melanosis Coli
Effective treatments are available to help patients who experience chronic constipation and bloating to develop regular bowel movements in a safe and sustainable way.
Do polyps of the colon cause symptoms?
Symptoms are highly unreliable predictors of the presence of cancer and polyps. If you are 50 years of age and older, you are encouraged to go for colon cancer screening independent of whether you experience symptoms or not. This is simply because age alone is a risk factor for colon cancer. People with a family history of colon cancer should start screening at an earlier age, either from the age 40 or ten years before the age at which their family member were diagnosed with colon cancer. Polyps in the colon, particularly the adenoma type, can be precursors of colon cancer. Fortunately, if polyps are discovered when they are small (eg less than 1cm) they are rarely cancerous, and can be readily removed at the time of a colonoscopy. In the event that polyps have been detected and removed, the interval before the next colonoscopy will be determined by the size and the numbers of polyps, and the types of cells found in a polyp. In general this can range from 6 months to 3 years.
Can adhesions, cysts and endometriosis in the uterus or ovary cause IBS symptoms?
We have to be very careful against blaming abdominal pain and bloating on adhesions and problems of the uterus and ovaries. One study from the UK showed that over half of women who had gone to see their gynaecologists for abdominal pain actually had symptoms of IBS. Of these women with IBS, the gynaecologist could only diagnose IBS in 16% of them. It has been repeatedly observed that women with IBS undergo more gynaecological surgery. It has been calculated that for every 1000 women with IBS there is an excess of 57 more hysterectomy than for women without IBS. One study from the US found that women with IBS who underwent laparoscopy or hysterectomy did not do as well as women without IBS, as they were more likely to continue being troubled by their symptoms. Another study from the US found that adhesions, ovarian cysts and endometriosis were just as common among women without any abdominal or pelvic pain as in those with pain.
The fact that a person’s pain is made worse by certain foods would suggest that the pain is coming from the digestive system not the uterus or the ovaries. The feeling of not completely clearing your bowels is also a sign of a bowel disorder. In women, bowel functions can vary with the time of the month, so that even if pain and bloating are worse around the time of the menstrual period, they can still be due to IBS. It is also possible that some women develop constipation after surgery to the uterus. Before rushing off for surgery, it is important to discuss with your doctor whether your symptoms could be due to IBS.
Does food poisoning or the use of antibiotics cause the development of IBS?
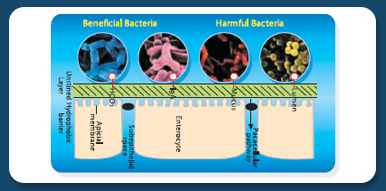
An episode of food poisoning or gastroenteritis is now recognised to be a major cause of IBS. In some patients with IBS, modern laboratory testing is able to demonstrate the presence of low grade inflammation in the intestine and even in the blood circulation. It is possible that exposure to harmful bacteria could trigger low grade inflammation which in turn could make the intestines more sensitive. Frequent use of antibiotics also appears to increase the risk of IBS. It is possible then that gastroenteritis or use of antibiotics could produce a change in intestinal bacterial flora. A number of studies have reported changes in the composition of bacteria found in the intestines of IBS patients, with some showing reduced numbers of bacteria such as lactobacilli and bifidobacteria.
Can probiotic bacteria help to improve bowel problems?
Some of these lactobacilli and bifidobacteria are potentially important to the health of the intestines as they support the immune system and supply energy to the intestinal lining cells. These good bacteria are known as probiotics derived from Greek and Latin words meaning ‘for life’. While findings are still preliminary, several studies suggest that probiotics may help to reduce symptoms of bloating and flatulence in IBS, reduce inflammation in the intestine, and also to prevent travellers’ and antibiotic-associated diarrhoea.
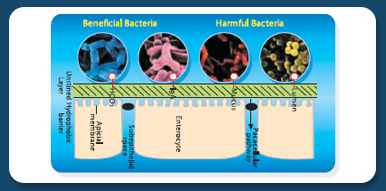
Probiotic and Gut Immunity
What is the difference between prebiotic and probiotic?
Another potentially useful approach is to supply key nutrients, known as prebiotics, that selectively support the growth of probiotic bacteria. In practice, prebiotics are composed of short-chain carbohydrates such as inulin and fructooligosaccharides, that are resistant to human digestive enzymes. In this way, they are able to reach the probiotic bacteria. These prebiotics are also known as colonic foods because probiotic bacteria will break them down to release short chain fatty acids (SCFA) which are important energy foods for the cells of the colon. SCFA has the potential to stimulate intestinal movements known as peristalsis, which play a role in normal bowel movements. Consumption of prebiotic has been reported to improve the bowel habit of chronically constipated people.
download Chinese version
PREVIOUS PAGE
|